Physical Readiness Assessment and staff resilience
Dr Alan Walmsley
Project Manager, Physical Readiness Assessment, Department of Corrections
Author biography
Alan was on the staff of the University of Otago and Massey University and has worked in the sport and exercise field in New Zealand for more than three decades. He is a life member and former Deputy Chair of Sport and Exercise Science New Zealand and a former council member of the International Society of Biomechanics. Alan has previous experience of occupational fitness assessment for the New Zealand Fire Service, and joined Corrections in March 2013 to design and develop the PRA.
Introduction
In response to staff expressing concerns about their safety in threatening situations, the expert panel on staff safety recommended that a Physical Readiness Assessment (PRA) be developed and introduced. The PRA project was initiated in March 2013 and, over the next year, the PRA was designed, and the constituent elements piloted, with the assistance of staff at Whanganui Prison. Subsequently, performance standards were determined from the results of a study undertaken at eight prison sites.
The PRA is intended to provide an indication of occupational physical performance in relation to the population of frontline staff. However, the PRA also indicates the general level of fitness of participants because performance in some elements of the PRA is dependent on aerobic and anaerobic fitness and muscular strength and endurance. The positive effects of physical fitness on the psycho-physiological stress response indicates that performance in the PRA could serve as a useful indicator of stress resilience.
Physical Readiness Assessment (PRA)
The elements of the PRA are based on the need for any assessment of occupational fitness to reflect the actual requirements of satisfactory performance in the job. Discussion of the physically demanding tasks performed by corrections officers provided the basis for selection of the various elements of the PRA, which were combined into a scenario that reflected a typical sequence of events:
A corrections officer is walking from one unit to another to conduct a search. During the search an emergency ‘Break – Break – Break’ call is received. The corrections officer runs as quickly and safely as possible to the scene of the emergency and has to use physical force to restore order. Once order is restored, the corrections officer notices an unconscious colleague, and so removes him/her to a place of safety for others to take over care. Once the emergency is dealt with, the corrections officer walks back to the original unit.
The PRA is composed of six elements; a 300m maximum speed walk, a simulated search, a simulated emergency response, simulated spontaneous ‘control and restraint’ (C&R), simulated rescue, and a 300m recovery walk. The time for the walking and running sections and the total time taken are recorded and generate scores. The simulated C&R score is determined from measurement of the maximum sustained horizontal force as a percentage of body weight. The five scores generated are combined to produce an overall score for the PRA which is used to determine the performance zone the participant will be placed in.
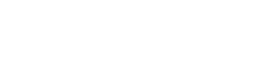
Prior to setting performance standards, the test-retest reliability of the individual elements and the overall PRA was estimated in a small sample of corrections officers. The volunteers completed the PRA on two consecutive days at the same time of day. Figures 1 and 2 indicate a high level of agreement between the scores from test 1 and test 2 and so the PRA was considered to be a reliable measure of occupational readiness.
Following the reliability study, 200 frontline staff completed the PRA as volunteers to allow performance standards to be set. Analysis of variance revealed small effects for both gender and age in all the variables. Further examination revealed that only participants over 60 were significantly different from all other age groups. These effects may be investigated in more detail in the future but, initially, neither age nor gender was considered in setting initial performance standards because the mean differences in measures were small (approximately equal to 5 percent). Performance scores were determined by converting the raw data to z-scores and placing participants in the ranges shown in Table 1. Each variable was scored individually, and the sum of z-scores was used to determine the final score. The number of participants falling in each score range is shown in Figure 3.
Figure 1
Overall correlation between variables from Trial 1 to Trial 2.
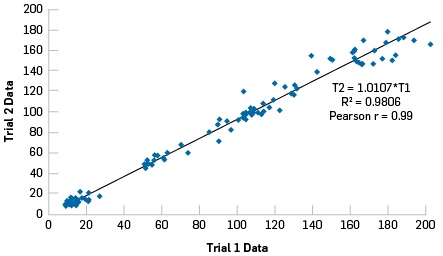
Figure 2
Bland-Altman plot of normalised data.
Figure 3
Number of participants falling into each score band.
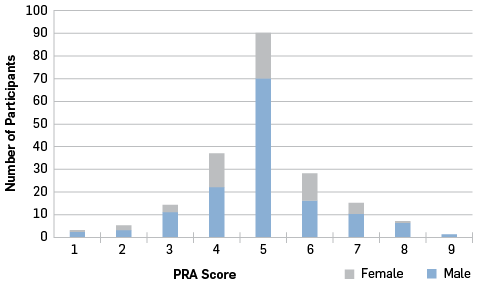
Table 1
Scoring ranges for measured variables
|
z-score |
PRA Score |
Description |
|
<= -2 |
1 |
WELL BELOW AVERAGE |
|
<= -1.5 |
2 |
|
|
<= -1 |
3 |
BELOW AVERAGE |
|
<= -0.5 |
4 |
|
|
>-0.5 to <0.5 |
5 |
AVERAGE |
|
>= 0.5 |
6 |
ABOVE AVERAGE |
|
>= 1.0 |
7 |
|
|
>= 1.5 |
8 |
WELL ABOVE AVERAGE |
|
>=2 |
9 |
Experience from other agencies and jurisdictions suggested that rather than a simple pass/fail approach the results from the various elements of the PRA should be scored. The scores place staff in a red (well below average), amber (below average) or green (average or above) zone. This approach is a more appropriate measure of fitness for the role because it places an individual in the population of corrections officers and also allows the individual to target training to specific elements that may be causing them issues.
Once performance standards were established, the PRA was trialled at Manawatu and Rimutaka Prisons to examine how the PRA might impact normal operations, how the confidentiality of PRA outcomes could be maintained, and how support could be provided to those staff who needed to improve their PRA performance. The trials finished at the end of September 2014 and, in addition to the planned outcomes, yielded some useful insights into staff reaction to the PRA and the associated administrative and support processes. Subjective assessment of the PRA as a measure of occupational performance was positive with all feedback confirming the expected high face validity. Most participants expressed the view that the PRA score reflected the ability of a staff member to keep themselves and their colleagues physically safe at work.
Figure 4
The dimensions of resilience and therapeutic interventions that affect them (Southwick & Charney, 2012).
|
Environmental stressors and genetic predisposition |
|||
|
Depression risk factors |
Therapeutic intervention |
Resilience protective factors |
|
|
Cognitive/behavioural |
Weak executive function: weak coping self efficiency; negative attention bias; cognitive inflexibility |
Cognitive behavioural therapy with cognitive reappraisal; positive emotion exercises; coping skill development, and training; well-being therapy |
Strong executive function: high coping self-efficiancy; positive emotions; realistic optimism; cognitive flexibility |
|
Emotion regulation |
Weak regulation (e.g., anhedonia; slow stress recovery) |
Mindfulness; training; antidepressant medications |
Strong regulation (e.g., delay gratification; rapid stress recovery) |
|
Social |
Weak social skills; minimal social network; no resilient role models |
Social emotional training; network support treatment |
Strong social skills; diverse social network; resilient role models |
|
Physical Health |
Sleep deprivation; poor cardiovascular fitness; poor nutrition; obesity |
Teach sleep hygiene; exercise regimen; improve diet |
Strong sleep habits; physically fit; good nutrition |
|
Neurobiology |
Dysregulated HPA axis and SNS in response to stress; attenuated prefrontal cortical executive function and stress-induced limbic system hyperactivity |
Neural circuit training; novel medications (corticotropin-releasing factor, NPY, GABA, glutamate) |
Effective regulation of HPA axis and SNS in response to stress; robust prefrontal cortical executive function and capacity to regulate limbic reactivity to stress |
How does the PRA help individuals to maintain or improve their resilience to stress? The PRA has always been seen as part of a general staff wellness system because it indicates an individual’s status in one dimension of wellness; physical fitness. Most practitioners recognise six dimensions of wellness, namely, physical, occupational, intellectual, social, emotional, and spiritual. Figure 4 indicates that all-round ‘wellness’ is closely linked to the resilience protective factors, and so, if resilience may be conceptualised as an adjunct to all-round ‘wellness’, any measure or indication of wellness could also indicate the resilience of the individual. Therefore, interventions that improve wellness may also affect resilience to stress. Data from the limited trials of the PRA suggest that it could be seen as an indicator of the physical and occupational wellness of participants, and so could be a useful tool in indicating individual resilience.
Stress and stressors
A stressor is an external stimulus or event that triggers a psycho-physiological protective response, and stress is the physiological response(s) to a stressor. For corrections officers, the most obvious occupational stressors are likely to arise from perceived physical or psychological threats, or events that occur while on duty. However, corrections officers, like all of us, are also subject to stressors arising from their home and personal lives that could have significant results in the workplace because of the need for vigilance and situational awareness while on duty.
Exposure to stressors will activate one or all of three physiological pathways that are responsive to psychosocial stimuli (Everly & Lating, 2002). In order of recruitment and intensity of response, the pathways are; the neural axes, the neuroendocrine axis, and the endocrine axes. The neural axes initiate the immediate physiological responses such as increases in blood pressure, dilation of the pupils, and inhibition of digestive functions; the neuroendocrine axis initiates the ‘fight or flight’ response including increased cardiac output and stimulation of skeletal muscles; and the endocrine axes determine chronic responses such as suppression of immune mechanisms. In general, the activation of these pathways depends on the intensity and duration of the stimulus, with the endocrine axes requiring much greater stimulus intensity and duration to initiate activity.
The ability to cope with stress (i.e. the psycho-physiological responses to the occurrence of a stressor) depends on the strategies used to attenuate the stress response. Coping strategies may be categorised as adaptive (reduce stress while promoting long term health) or maladaptive (reduce both stress and long term health). Physical exercise, good sleep habits, and good nutrition may be seen as adaptive coping mechanisms, while alcohol or drug abuse and social withdrawal may be seen as maladaptive mechanisms (Silverman & Deuster, 2014).
Excessive or prolonged stimulation of the physiological pathways may result in organ dysfunction or pathology. This process, known as target organ activation, and the subsequent clinical signs and symptoms are the clues we use to deduce the presence of stress induced illness.
Resilience
Resilience to stressors is a complex multi-dimensional construct, which encompasses the processes of adaptation to adversity and physical threat. To understand the links between stressors, stress, interventions such as the PRA, and resilience it may be helpful to have a common definition of resilience; I will use the US Air Force definition "the ability to withstand, recover from, and grow in the face of stressors" (Robson, 2013).
As an exercise scientist, I conceptualise resilience in terms of the ability to deal positively with repeated episodes of the physiological responses to stressors; that is, coping mechanisms are adaptive. The brain is the key organ of the stress response because it is here that the perception of threat is interpreted and the subsequent physiological response integrated and organised (McEwen, 2007). Neural and endocrine mechanisms mediate the communication between the brain and other organ systems that organise and mount both the acute and chronic stress response. There is some evidence that habitual exercise may benefit brain function by enhancing the effects of growth hormone on neural structures, which improves cognition (Silverman & Deuster, 2014).
There is abundant evidence that habitual participation in physical activity is linked to better health throughout life; more active individuals have lower rates of coronary artery disease, hypertension, stroke, type II diabetes, metabolic syndrome, and depression (Salmon, 2001). The evidence also indicates that an increased level of habitual physical activity ameliorates the target organ effects of the stress response by reducing stress sensitivity; fitter individuals exhibit reduced physiological reactivity to stress and faster pulse rate recovery. Furthermore, the effects of stress reduce as physical activity is increased over time. Physical activity has many direct and indirect benefits to the health, well-being, and readiness of frontline staff:
It is strongly linked to better medical fitness (e.g., cardiorespiratory health, reduced risks for some cancers), physical fitness (e.g., body composition, muscular fitness), psychological fitness (e.g., stress-buffering, protection against depression and anxiety, increased self-esteem), and behavioral fitness (e.g., good sleep practices, sleep quality). Physical activity can also help reduce the major risks to optimal mission performance: physical injury, being overweight and psychosocial dysfunction. Furthermore, group physical activity can improve social fitness through the development of social networks and cohesion (Robson, 2013, p. 23).
Conclusion
The PRA is an indicator of physical and ocupational fitness, and improving performance in the PRA by being habitually physically active will help confer resilience by reducing stress reactivity and the behavioural and metabolic consequences of stressful episodes. Assisting staff to be physically active and maintain and enhance their physical fitness will pay dividends in terms of resilience to stress.
The contributions of physical fitness to resilience make it a smart investment, even in times of scarce resources (Robson, 2013, p. 24).
References
- Everly, G. S., & Lating, J. M. (2002). A clinical guide to the treatment of the human stress response. New York: Springer Science.
- McEwen, B. S. (2007). Physiology and neurobiology of stress and adaptation: central role of the brain. Physiol Rev, 87 (3), 873-904. DOI: 10.1152/physrev.00041.2006.
- Robson, S. (2013). Physical Fitness and Resilience: A Review of Relevant Constructs RAND Project AIR FORCE Series on Resiliency (pp. 32 pages). Washington DC: RAND Corporation.
- Salmon, P. (2001). Effects of physical exercise on anxiety, depression, and sensitivity to stress: a unifying theory. Clinical psychology review, 21(1), 33-61.
- Silverman, M. N., & Deuster, P. A. (2014). Biological mechanisms underlying the role of physical fitness in health and resilience. Interface focus, 4(5), 20140040.
- Southwick, S. M., & Charney, D. S. (2012). The Science of Resilience: Implications for the Prevention and Treatment of Depression. Science, 338, 79-82.