A mental health service for people in central North Island prisons
Shaun Sullivan
Project Manager, Waikeria Mental Health Service Project, Department of Corrections
Maxine Mallinson
Senior Policy Adviser, Strategic Policy Team, Department of Corrections
Author biographies:
Shaun, LLB, BA(Hons), PRINCE2 Registered Practitioner, previously worked for Police and Ministry of Social Development, before joining the Department of Corrections Design & Implementation team in mid-2017.
Maxine, LLB, BA(Hons), joined Corrections in early 2017. Maxine previously worked as a lawyer in a general practice role, primarily focused on litigation.
Background
In 2018, the Department of Corrections (Corrections) commenced the development of a 600-bed facility at Waikeria Prison, due for completion in 2022. The government announced that, due to the high proportion of prisoners with mental health issues, 100 of the beds in this facility would be dedicated to a mental health service. This will be the first service of its type in a New Zealand prison.
People in prison have a high prevalence of mental health conditions compared with the general population, with a significant degree of co-morbidity with substance abuse and neuro-cognitive issues. A recent study indicated that 91 percent of people in prison are likely to have met the criteria for a mental health or substance abuse diagnosis within their lifetime. A subset of 62 percent had received a diagnosis within the preceding 12 month period (Bowman, 2016).
In recent years, Corrections has strengthened its provision of mental health support to people in prison through:
- Mental Health and Reintegration Services provided by mental health clinicians in 16 prisons and four Community Corrections sites
- A new model for our Intervention and Support Units, centred on a more therapeutic, multidisciplinary approach for people who are vulnerable to suicide and self-harm.
The Waikeria mental health service will build on these investments and strengthen Corrections’ ability to provide specialist services. Specifically, a person-centred approach will be implemented in a health-focused environment, to support the rehabilitation of men with a mental health diagnosis, alongside therapeutic support for other complex needs.
The development of this service presents an opportunity to work in partnership with Māori, the Waikato District Health Board (DHB) and the Ministry of Health. A joint approach with our partners promotes best practice, draws on our respective strengths, and will increase the likelihood of successful outcomes.
A project team has been established to design, develop and implement an operating model for this facility.[1] A collaborative approach will drive the development of an operating model, with the aim of incorporating several focuses:
- integration with the rest of the prison network and the wider mental health sector, including strong referral pathways
- a strong kaupapa Māori approach at the centre of the model
- providing therapeutic support and rehabilitation where needs cannot be met in mainstream prison units
- a person-centred approach that is responsive to needs.
The wider mental health context
The development of this mental health service requires consideration of the wider health context, including the role of forensic mental health services, and the response to the report of the Government Inquiry into Mental Health and Addiction, He Ara Oranga.
In November 2018, He Ara Oranga made recommendations aimed at improving New Zealand’s approach to mental health. Areas of focus included equity of access, community confidence in the mental health system and delivering better outcomes for Māori. He Ara Oranga said that in an aspirational future state:
“There will also be stronger connections and capability within forensic services for specialist psychiatric liaison into prisons for people who are incarcerated, and the capacity to more easily transfer people who are very unwell into a health-focused environment” (Mental Health Inquiry, 2018).
In this respect, the Waikeria mental health service will be additional to, and not a replacement for, the services that are delivered by the Waikato DHB. Forensic mental health facilities will continue to provide specialist treatment and rehabilitation to people who meet the criteria for admission, and compulsory treatment will not be provided within Waikeria Prison.
However, there are significant constraints on the capacity of forensic mental health services, as highlighted by He Ara Oranga. In particular, the growth of the prison population has not led to a corresponding increase in the volume of forensic mental health beds (Skipworth, 2018).
Working within this context, the Waikeria mental health service will provide therapeutic support after people return to prison from the Midlands forensic mental health facility. After people return from this facility, they typically present with a lower level of acuity, but tend to require ongoing mental health support and rehabilitation to reduce the likelihood of re-admission.
The international context
Internationally, an evidence base is developing that outlines the importance of mental health screening and triaging within prisons, to support effective treatment (Skipworth, 2018). In this respect, a number of Australian jurisdictions have developed specialist mental health services within prisons, with a particular focus on triaging and screening processes.
Caution needs to be exercised about overseas models, as we cannot assume they will be applicable in the New Zealand context. Overseas models reflect their particular corrections environments, health sectors and cultural milieu, which differ from those in New Zealand. However, the project team will consider these international models – to understand the challenges of developing this type of unit in a prison environment and to help guide the development of the Waikeria mental health service.
In particular, we will draw from the examples of prison-based mental health services in New South Wales (NSW) and Victoria, Australia. Both jurisdictions place significant emphasis on initial mental health assessments and screening, which is followed by specialist care in the prison. In reality, there are significant differences in the delivery of services in these jurisdictions, which reflects different legislative frameworks, philosophical approaches and cultural imperatives.
For instance, in NSW compulsory treatment can be delivered within a designated hospital inside a prison (Mental Health Act (NSW) 2007). In contrast, Victoria’s legislative framework precludes the delivery of compulsory treatment in a prison setting, which means that prison-based services must be integrated with an external forensic mental health facility (Mental Health Act 2014 (Vic).
In New Zealand, Corrections delivers primary health services to people in prison, and secondary and specialist services are delivered by DHBs and contracted providers. In the mental health sector, local DHBs run the five Regional Forensic Mental Health Services that deliver services for people within the justice sector.
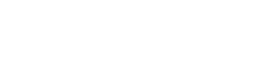
Hence, New Zealand’s structure differs from NSW and Victoria, which have developed distinct entities to deliver primary healthcare and forensic mental health services. In NSW, a specialist unit called Justice Health was formed a couple of decades ago to deliver all prison-based health services, and forensic mental health services across all justice-sector settings.
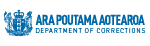
In contrast, Victoria has developed a specialist unit to deliver primary healthcare, also referred to as Justice Health, and delivers forensic mental health services through a sub-unit called Forensicare. Forensicare was formed under Victoria’s mental health legislation, and delivers mental health care to people in the justice system in accordance with its statutory duties (Mental Health Act 2014).
Both these agencies have been embedded in the justice and health sectors in these jurisdictions for many years, with a single provider addressing mental health across the prison estate and in external forensic mental health services
Additionally, within NSW and Victoria, there is a network of mental health facilities across the prison estate, so that assessment and screening units feed into more substantive prison-based facilities in each state. A high level overview of these models is set out in Appendices One and Two.
Culturally responsive services provided in the Mason Clinic
To ensure that the Waikeria mental health service is informed by the New Zealand context, the project team has partnered with regional forensic mental health services, the Ministry of Health and mana whenua to draw from kaupapa Māori frameworks in the wider health sector.
Collectively, these examples will inform the design of a health-centred, culturally-responsive operating model that meets the needs of our people. Consideration will be given to developing integrated and therapeutic pathways to meet needs during transitions, such as upon release or during transfers to different environments within the prison network.
Previous experience in the health sector indicates that services must be culturally responsive to meet needs effectively. The Mason Clinic’s Te Papakainga o Tane Whakapiripiri and Te Aka units deliver kaupapa Māori services in a forensic setting, and are pioneering examples of this approach.
These units were established in response to over-representation of Māori in forensic mental health services. From the outset, the vision for Te Papakainga o Tane Whakapiripiri and Te Aka units was to provide a range of clinical and cultural services that will improve mental health outcomes for patients, whānau, hapu, and iwi. Crucial features of the development of these services were:
- a new model of care, with broad consultation, and clinical and cultural involvement at all stages of development
- recognition of the unique opportunity, and of the importance of getting it right.
Māori, who make up 15 percent of the general population, account for 45 percent of the forensic mental health population (Ministry of Health 2007), 52.9 percent of the prison population, and 73.3 percent of the population at Waikeria Prison (Corrections, 2019). Key relationships have been established with the Mason Clinic, which forged the pathway for kaupapa Māori services to be delivered in a forensic setting. These relationships will support and guide the development of the Waikeria mental health service operating model.
Forensic mental health services in the central North Island
Additionally, the relationship with the Henry Rongomau Bennett Centre, the Hamilton-based regional forensic mental health service known as Puawai will be critical to the Waikeria mental health service. Puawai provides services across four DHBs in the central North Island.[2] The relationship is twofold in that we can learn from this service and have partnered with the Waikato DHB, which will have significant involvement in the operational aspects of the Waikeria mental health service.
In 2010, the Waikato DHB centred the newly configured Puawai service on:
“healing, growing and celebrating a partnership between an agency of the crown and a kaupapa Māoriorganisation moving forward together as one” (Waikato DHB press release, 2010).
Currently, Puawai consists of a 44-bed secure inpatient services, court services, outpatient prison-based services, and community follow-up services in Hamilton. Puawai, and other services run by the five DHBs, will be critical to ensuring effective continuity of care for people moving through the Waikeria mental health service, including on release from prison.
Puawai will provide a pathway when a person’s level of mental health acuity escalates beyond the type of care that will be provided by the Waikeria mental health service, such as when compulsory treatment is required under the Mental Health (Compulsory Assessment and Treatment) Act 1992. Equally, the Waikeria mental health service will provide a therapeutic pathway for when people are well enough to return to prison from forensic mental health services.
Key workforce challenges
In 2014, Te Pou (the national centre of workforce development for the mental health, addiction and disability sectors) surveyed 7,613 employees in the adult mental health workforce across New Zealand. Survey responses suggested that a number of clinical and allied health roles were at risk of future shortages, including nurses, consultant psychiatrists, clinical psychologists, occupational therapists, and support workers (Te Pou, 2014).
These findings were reflected in the report He Ara Oranga, which pointed to major issues with the recruitment and retention of staff, including negative perceptions about working in mental health. The report noted that these issues place pressure on existing staff, and will impact future recruitment (Mental Health Inquiry, 2018).
The opening of the Waikeria mental health service will add pressure to the workforce in this sector, with particular reference to two critical factors that impact our ability to develop and operationalise a skilled workforce:
- known workforce shortages in the adult mental health sector
- large scale recruitment into a rural setting (given that the prison is 16km south of the small town of Te Awamutu).
To effectively respond to these challenges, the agencies involved will focus on growing the current workforce, which includes implementing strategies that are both innovative and evidence based.
Ensuring continuity of care
Ensuring continuity of care and integration with other services will be a critical aspect of this facility. He Ara Oranga highlighted the need to reduce fragmentation within the wider mental health system, which has a significant impact on many Māori communities (Mental Health Inquiry, 2018). In particular, integration with community-based adult mental health services will be an important part of ensuring continuity of care after release.
Within the prison environment, people require “step-down” services to facilitate recovery from a period of being acutely unwell. Step-down services will offer support after people transition from acute care in Forensic Mental Health Facilities, during a period when they need ongoing rehabilitation but their needs are less acute. The need for an improved continuum of support was reflected by tāngata whaiora, families, whānau, clinicians and NGOs (Mental Health Inquiry, 2018).
An agreed approach to continuity of care will provide a robust platform for broader sector responses in the central region. The development of an operating model will be used as a platform to drive integration within the wider sector, in partnership with the Waikato DHB and the Ministry of Health, including:
- a therapeutic and recovery-focused model of service delivery
- effective governance and decision-making, involving Corrections, the health sector and Māori
- ensuring that the model interfaces with the rest of Waikeria Prison, other prisons, and other forensic and community mental health services
- a comprehensive workforce development plan.
The mahi to develop the operating model is underway
The successful development of a person-centred, culturally-responsive operating model should improve mental health outcomes for men imprisoned in the central North Island.
A project team based in Wellington and Hamilton has been established to design and develop an operating model for this facility. Key project deliverables will be reviewed and endorsed by an advisory panel comprised of subject matter experts from Corrections, service users, and cultural, clinical, and academic fields. Once endorsement has been received, all key decisions will be made by a cross-agency Project Board with representation from Corrections, Waikato DHB, Ministry of Health, Te Puni Kōkiri, and iwi.
References
Bowman, J. (2016). Comorbid substance abuse disorders and mental health disorders amongst New Zealand prisoners. Practice, The New Zealand Corrections Journal, Vol 4, Issue 1, August.
Department of Corrections, Research and Analysis Team, as at 28 February 2019
Mental Health Inquiry (2018). He Ara Oranga: Report of the Government Inquiry into Mental Health and Addiction (https://mentalhealth.inquiry.co.nz).
Ministry of Health (2007). Census of Forensic Mental Health Services 2005. Wellington: Ministry of Health
Skipworth J. (2018). The Australian and New Zealand prison crisis: Cultural and clinical issues. Australian and New Zealand Journal of Psychiatry.
Te Pou (2014). Adult Mental Health Survey: 2014 Survey of Vote Health Funded Services (https://www.tepou.co.nz).
Waikato District Health Board (2010). A New Start for Forensic Service, Patients (http://www.scoop.co.nz).